A
A
A
If you are like many of us, you are struggling to balance your life and make the appropriate decisions to protect the health of your family. The school year is right around the corner and the news is flooded with reports of record numbers of new infections.
With over 14 million people infected and more than 600,000 global deaths, a mere 6 months since COVID-19 was first reported, herd immunity may be the key to bringing an end to this global pandemic and restoring some normalcy to our lives. There are two ways that people can become immune to the virus; contracting the virus and vaccination.
However, these methods are only effective if they produce a lasting immune system response to ward off future infections. That’s why everyone wants to know how long you are immune to COVID-19 after infection or vaccination.
To answer this, we need to look into how the immune system kills viruses and how
vaccines may work to bring an end to the current pandemic.
The Immune System
Your immune system is responsible for identifying and destroying infections in the body. T-cells, which are developed in the thymus, identify a virus or infection in your body and signal b-cells, which are produced by the bone marrow, to produce antibodies to neutralize the virus before it infects healthy cells. However, these antibodies are just one part of your body’s immune system response.
Whereas b-cells produce antibodies to neutralize viruses before they can infect healthy cells, some t-cells, called cytotoxic t-cells, use special proteins to identify infected cells and kill the infected cell before the virus infecting it it can spread.
Viruses adapt quickly and can trick the t-cells into not recognizing it. That means that the immune system may overlook it and allow it to spread. If the immune system doesn’t recognize a virus, it can spread quickly through the cells of the body.
It takes time for the immune system to identify, target, and appropriately attack a new virus. As the virus reacts, it can quickly change how the immune system remembers and responds to it.
Immunity occurs when your body’s immune system recognizes a virus and responds quickly to kill it and the infected cells before they spread and you become ill.
Developing Immunity
Read More »
To develop an immune response against a virus, your body needs to have antibodies and t-cells that recognize the virus. Your body can create antibodies if it has been ingected or has received a vaccine.
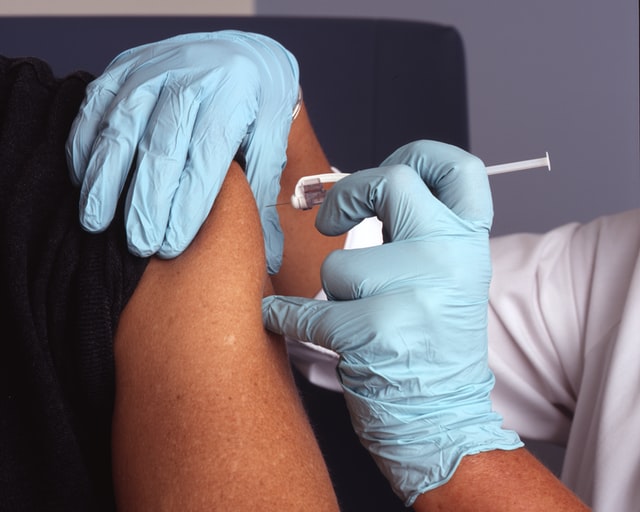
Vaccination is the least dangerous of these two options. With vaccination, a weakened or dead version of the virus is injected or inhaled by a person. The weakened virus isn’t strong enough to make you ill, but it triggers your immune system to recognize and attack it.
This allows your body to produce t-cells and antibodies that recognize the virus should you come into contact with it in the future. Once infected with the virus, your immune system will recognize the threat quickly and neutralize it before it becomes a serious illness.
While some people develop symptoms with vaccination, they are far milder than the actual illness and you will not be contagious. Contracting the actual virus leads to more severe illness and the patient will be contagious to others.
Immunity is important because it allows our bodies to react more quickly and head off the infection more effectively. This can prevent infection in many people and reduce the severity of your symptoms should you develop an infection. This saves lives and valuable resources.
How Long Are You Immune to COVID-19?
Right now, we really don’t know how long people are immune to COVID-19. While multiple vaccines are in the works, the virus is so new that there isn’t enough data to go on. All we can do is look at the limited data and draw potential conclusions.
A recent study conducted by researchers at King’s College London indicates that most antibodies may only be present for several weeks after infection, especially in people who only developed mild symptoms. However, people who developed a more severe illness kept antibodies much longer.
This can seem disheartening, but it doesn’t look into the full immune system response to the illness. The King’s College London study didn’t look at T-cells, another very important factor in becoming immune to COVID.
More studies are needed and are currently being conducted to determine how the entire immune system responds after we have been exposed to the virus.
T-Cells and COVID-19
T-cells can identify and attack a virus much longer than antibodies can live in our system. Without significant research on COVID, we can look at studies completed on both SARS and MERS. These coronaviruses are closely related to COVID but were more deadly and less contagious.
According to research performed in Singapore on monkeys, memory t-cells responded to the SARS virus nearly 17 years after the monkeys were originally infected with it. This long-lasting immunity is promising for the COVID vaccines and indicates that although antibodies are short-lived, we may be able to obtain a longterm immune response thanks to those memory t-cells.
However, it is important to note that this data is not conclusive since the research wasn’t conducted on the same virus and it wasn’t conducted on humans. Right now, we can only determine if a person has had COVID if they have antibodies in their blood and how long those antibodies lasted in the patients who have contracted the virus.
It may be years before we can understand how t-cells respond to a second COVID infection. If t-cells recognize the virus for an extended period of time, not only can it prevent infection, it can greatly reduce the severity of the infection. Preventing the severity of infection will save lives and minimize the longterm side effects of the virus.
Returning to normal may be right around the corner with a new vaccine being tested and mass-produced right now. It will be interesting to see how long antibodies last and t-cells can recognize the virus and protect us from the infection.